Turning Healthcare Claims Data into Actionable Insights
Objective to demonstrate how Power BI dashboards can transform medical claims data into actionable insights by analyzing claims, denials, financial performance, and procedure costs — enabling healthcare organizations to improve efficiency, reduce revenue leakage, and make informed decisions.
Project Overview
The client is a healthcare provider managing a large volume of claims across multiple insurance types. They struggled to track claim statuses, understand denial trends, and monitor reimbursement rates efficiently. Their goal was to gain end-to-end visibility of claims data and improve revenue cycle management.
Challenge
Fragmented and siloed claims data spread across systems.
Difficulty in identifying top denial reasons and recurring claim issues.
Lack of visibility into financial performance — billed vs. paid amounts and reimbursement rates.
Limited insights into the cost impact of procedures and their utilization.
Time-consuming manual reporting, leaving little room for strategic planning.
Our Solution
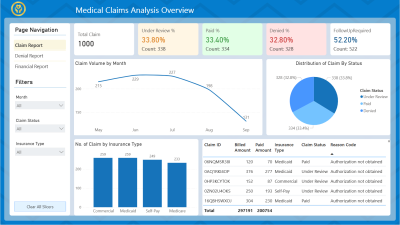
We developed an interactive Medical Claim Analysis Dashboard in Power BI with multiple reporting layers:
Claim Report
Overview of total claims, status breakdown (paid, denied, under review), and insurance type trends.
Denial Analysis Report
Identification of denial reasons, denial rates by insurance type, and month-wise denial trends.
Financial Performance Report
Detailed tracking of billed, allowed, and paid amounts with reimbursement rate analysis.
Procedure Analysis Report
Insights into top procedures by billed amount, utilization, and reimbursement impact.
Impact & Outcome
Reduced time spent on manual claim reporting by 40%.
Identified top denial reasons (e.g., incorrect billing, missing documentation) to reduce future rejections.
Improved visibility of reimbursement rates, helping optimize insurance negotiations.
Clear understanding of procedure-level financial impact, enabling better resource allocation.
Enhanced transparency and faster decision-making for finance and operations teams.
Report / Screenshots
Interect with the live dashboard below.
Technology Stack
- Power BI Desktop & Service – Dashboard creation, sharing, and automation
- DAX (Data Analysis Expressions) – KPI calculations and logic
- Power Query – Data cleaning and transformation.
- MySQL Server – Raw data source integration
Ready to unlock similar success for your organization?
Let’s discuss how we can help you achieve similar results with a custom Power BI solution.
